As payers look for innovative ways to improve care at a lower cost, Cigna and Elevance Health (formerly Anthem) are exploring opportunities in digital therapeutics.
Digital therapeutics (DTx) — which aim to treat, manage, and prevent diseases and disorders using evidence-based, clinically tested software — are gaining traction as a way to increase access to care while extending providers’ and payers’ ability to monitor patients.
For payers, the tech represents an opportunity to provide plan members with a 24/7 solution to address ongoing health issues. As more members transition to value-based care models, payers are looking to DTx to support patients in maintaining their health across care settings.
FREE DOWNLOAD: THE COMPLETE DIGITAL HEALTH 150 LIST
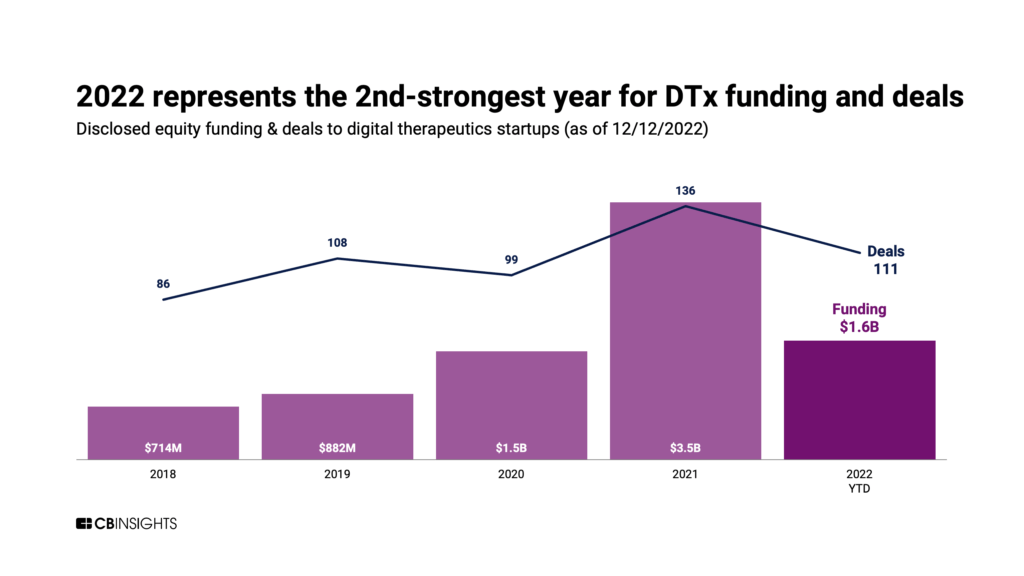
Inroads are being made across the DTx market. While not reaching 2021’s record highs, digital therapeutics providers have raised $1.6B in 2022 YTD across 111 deals — the second-highest levels ever reached.
While DTx adoption has been relatively slow to date, a handful of payers have started to cover prescribed digital therapies as part of a patient’s claim.
In particular, Cigna and Elevance Health — two of the largest payers in the US — have led the way. Cigna (via its Evernorth health services business) established a first-of-its-kind digital health formulary in 2019 to provide coverage for approved digital therapeutics, while Elevance drew up a clinical utilization management guideline in 2020 to define digital therapies and their coverage.
Below, we dig into what Cigna and Elevance Health are doing in the digital therapeutics market.
What are Cigna and Elevance Health doing in digital therapeutics?
Cigna and Elevance Health are both actively engaging with digital therapeutics companies to enhance chronic disease management and mental health treatment.
Want to see more research? Join a demo of the CB Insights platform.
If you’re already a customer, log in here.